Blogs & News
We Are in the ‘Age of Diabetes’
This week Diabetes Scotland released its 2015 State of the Nation report – it’s annual review of diabetes care in Scotland. As always, it makes for a fascinating, yet shocking, read. In the foreword alone we learn that ‘Scotland has the worst record of HbA1c control in the western world.’[1] In a wealthy nation with an excellent healthcare infrastructure, this is an alarming statistic. So what can be done about it?
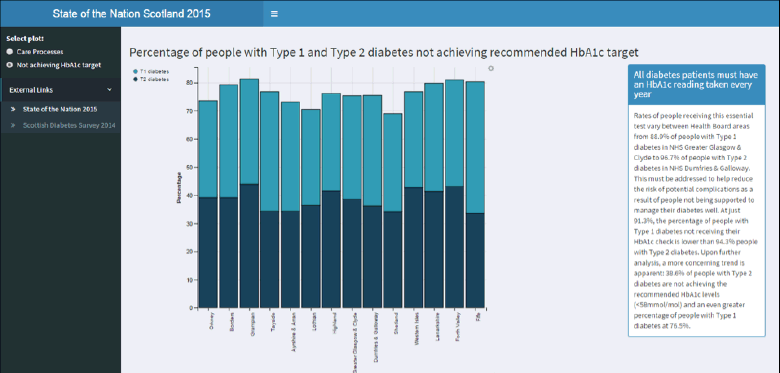
This AnalytiXagility mini-app demonstrates high numbers of patients not achieving the recommended HbA1c target
Scotland has one of the best integrated shared electronic patient records to support treatment of patients with diabetes (SCI Diabetes) in world; however, despite it being readily available to clinicians across the NHS, it is clear that much more needs to be done to tackle the rising tide of diabetes. Crucially, we must ensure that everyone diagnosed and living with diabetes receives the best possible care, irrespective of where they live.
Diabetes Scotland is right when it writes that ‘our access to information gives us power’ and that ‘information only matters if you use it inform positive change and better health outcomes’,[2] which is why NHS Scotland can – and should – be doing more with its rich and integrated diabetes data.
The application of SIGN’s nine care processes[3] is more than just a monitoring requirement or a tick-box exercise; evidence demonstrates that receiving these checks can postpone the onset of complications.
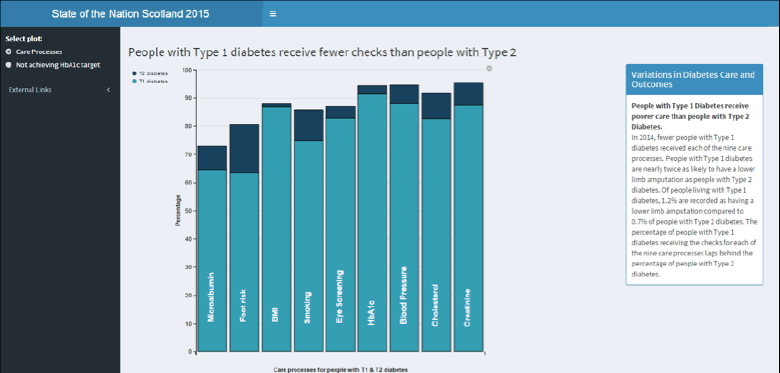
The State of the Nation report shows that Type 1 diabetics are receiving fewer checks and have poorer outcomes than Type 2 patients
In the short-term, the NHS should look at ways of using its data better to assist with both improving the consistency of diabetes care across Scotland, and reducing avoidable complications. One approach would be to take a data lake approach to bring data together and employ agile analytics to help the NHS understand its population more effectively, and adapt and change as circumstances change.
By more effectively using the high-quality data that already exists, employing advanced analytical techniques, and adopting the latest SaaS infrastructure, NHS Scotland has the potential to tackle this problem of unwarranted variation in diabetes care and improve patient outcomes across the country.
This notion of data science/agile analytics applied to healthcare, or data-driven medicine as it is also known, is the art of combining silos of related data and refining it into actionable insights that can be easily interpreted and visualised through interactive dashboards, or developed into data products or apps. To maximise the potential impact from these dashboards and apps, they need to work in near real-time, providing useful and reliable insights at the point of care and to end users – both healthcare professionals and patients.
For example, a focus on timely access to risk-factor profiling insights could enable early preventive care strategies to be implemented, reducing subsequent complications and costly hospital admissions.
Deploying analytics into the NHS brings the potential to shift the care of diabetes in Scotland from an acute model to a wellness model, where patients maintain optimal control of their condition and reduces the economic burden of managing the prevalence and outcomes of the disease.
Using data-driven medicine to support the effective management of diabetes and other chronic conditions should not only be seen as desirable, but as a necessary and logical way to ensure optimum health of a population. As costs spiral, and increasing numbers of Scottish patients fail to get even the minimum level of care, surely it is time to take a different, more data-driven approach.
September 3, 2015
Karen O'Hanlon
Engagement Manager
Karen is one of the main sources providing healthcare strategy and policy advice to the Aridhia team, keeping us up to speed with current healthcare trends and initiatives. She spends time horizon scanning, keeping her eye on what’s happening globally in healthcare and health informatics, and looking for business synergies and new opportunities. As key member of the business development group, Karen has an MBA and spent over 20 years working in the public sector. Prior to joining Aridhia she spent 12 years working on strategy and policy development for the Scottish Government.
